Brigette's Story
06 June, 2021
It was the worst of circumstances. A not-quite 28-year-old woman - newly relocated, unemployed, and uninsured - feels a small lump on her left breast.
Two weeks later she has a mammogram, followed minutes later by an ultrasound. “The technician is taking lots of pictures and says, ‘I’m going to get the radiologist.’ The radiologist enters the room and almost without preamble says, ‘I think you have breast cancer and you should start researching financial assistance and other means of support.’”

The temporary daze of the next few days would belie what has become a life’s work on behalf of cancer patients. Forged in the fire of two breast cancer diagnoses – one at 27 and another at 38 less than a month after giving birth to her son – Brigette Cole is both cancer survivor and patient advocate, for herself and for the thousands of Nevada women who also will hear the dreaded words, “You have breast cancer.”
As a Program Manager at Nevada Cancer Coalition, Cole helped lead the Northern Nevada Breast Cancer Collaborative to recommend uniform breast cancer screening guidelines based on a woman’s personal risk assessment. In a first for the Nevada breast-health community, a diverse group of the region’s leading healthcare providers announced Wednesday, October 2, 2019 at the Paint Nevada Pink event, their commitment to unified recommendations in how women are guided to breast cancer screening based on their age and personal risk assessment.
One week after her 28th birthday, Cole underwent surgery – a lumpectomy – to remove a small tumor, later diagnosed as Stage 1, Grade 1, infiltrating ductal carcinoma. Because of her youth, she was told she must begin aggressive chemotherapy within weeks, and to plan on dealing with its many side effects, including hair loss.
Cole’s foray into the dizzying world of cancer care had begun. Her first impressions weren’t what she might have hoped for.
Advocating, investigating for herself
“The healthcare world was cold,” she said. “People would look at me with an expression that read - you’re young, you don’t have resources - and they blew me off because of that. I don’t want to say they were judging me, but I was young, I was uninsured and they were like - too bad for you.”
Cole was angry, for all the many reasons.
She’s always been a get-it-done kind of woman. Though she was currently unemployed and felt that her doctors considered her a transient, she was in fact a college graduate with a bachelor’s degree in art. She’d been a wilderness ranger and a wildland firefighter, and she knew what it was like to face a firestorm.
She started researching and found financial assistance resources, enrolled in a medical discount program offered through a brand-new nonprofit called Access to Healthcare Network, and she got a job waitressing and bartending. Into the wee hours of the morning she searched the internet for treatment alternatives to chemotherapy, which scared her; and then she found a clinical trial that sounded promising.
“My grandmother had participated in a clinical trial for ovarian cancer and I always thought clinical trials were amazing because you get cutting edge treatment at no cost,” she said.
Three days before she was to start chemotherapy, she received word that she’d been approved for a clinical trial that was nearing approval for widespread use. Its effectiveness had been established. So now, in addition to the surgical lumpectomy, her cancer care would involve not chemotherapy, but six weeks of radiation treatment followed by an indeterminate course of treatment with the breast cancer drug Tamoxifen, an estrogen receptor blocker.
She drove herself to 7 a.m. radiation treatments every weekday, arriving along with a similarly-scheduled group of Nevada state inmates. It’s a little ironic that Cole’s first foray into cancer care advocacy began with her helping commission an art installation and benefit show for cancer survivors using the mesh ‘cancer cage’ silhouettes she saw while lying on the treatment table. One might imagine the cages as prison bars, though they are potentially life-saving.
It was the connection Cole made with the radiation oncology nurse who helped provide her care that began to change Cole’s initial impression of a healthcare system that felt out of touch with compassion, and made her determined she wanted to join in to help.
Getting on with life
Within weeks of completing her treatment, Cole began working for a local neurosurgery practice. A year later during a chance meeting with the CEO of Access to Healthcare Network (AHN), Cole told her she wanted to work for them. Cole was one of the first AHN cancer patients, and as a Care Coordinator at AHN she used her personal experience to help clients navigate the often confusing maze of receiving and paying for cancer treatment.
Meanwhile, she was dealing with side effects associated with Tamoxifen, including developing severe endometriosis. She underwent two surgeries to treat the disease and had one ovary removed. At 30, her doctors were talking about a hysterectomy. Instead, Cole chose to stop taking Tamoxifen, against the recommendation of her oncologist. The symptoms improved. When she sought a second opinion from a specialist about the possibility of having a child, she learned that pregnancy is an effective way to bring endometriosis under control. She’d always wanted and expected that she would become a mother.
But life had its own agenda, and within two more years her mother was diagnosed with a rare form of leukemia from which she passed away two months later.
“As a young breast cancer survivor you feel forever that you are damaged goods,” Cole explains. “That’s how I felt. I didn’t feel as though I was ever going to be able to have the happy healthy family I so dreamed of."
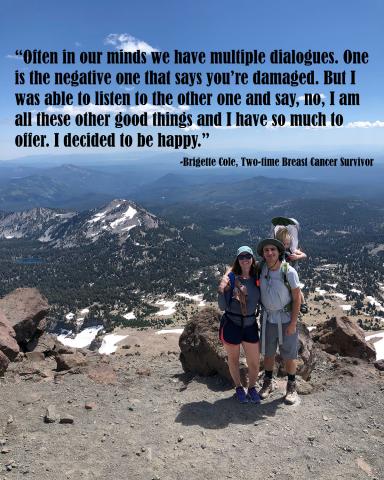
“Often in our minds we have multiple dialogues. One is the negative one that says ‘you’re damaged.’ But I was able to listen to the other one and say ‘NO! I am all these other good things and I have so much to offer.’ It’s like you have to choose which dialogue wins. And I decided that I'm going to be happy! I seized on that and started to leave all the negative behind me.”
She connected with a former colleague and they began a year of outdoor exploration across Nevada, running half marathons together, hiking every peak, and camping every weekend. Before long, they were in a deeply committed romantic relationship.
It was a joyous time. Cole stepped slightly away from her regimen of cancer care follow up - she stopped getting her regular mammograms for almost two years.
“I just didn’t want to take time. I wanted to be normal. I wanted to have the little piece of not being broken. And it was so healing. It filled all those things for me that I’d been missing.”
The couple began actively trying to become pregnant and within a few months it happened. “I was the happiest pregnant woman around. I was just glowing.”
Her pregnancy was uncomplicated and Cole’s biggest hope – that she would be able to breastfeed her baby – was realized.
Now what?
“Things started off great, but within two weeks my son never wanted to nurse from my left breast,” Cole recollects. “I saw the lactation consultant numerous times and was pumping so that I’d continue to have milk in both breasts. My baby definitely didn’t want to nurse on that side, and my breast was kind of lumpy. We felt what seemed like a little spot.”
After delaying for a couple weeks, Cole had a breast ultrasound. In an eerily familiar sequence, the ultrasound technician announced she was bringing in the radiologist. This time, the doctor told her he couldn’t say if the spot was cancerous. Within a week Cole had a biopsy and the result was very similar to before: Stage 1 infiltrating ductal carcinoma, located in essentially the same place as the first tumor. This time, she was referred to a breast surgeon for a mastectomy.
As before, Cole began researching. She soon knew the type of mastectomy and reconstructive surgery she wanted. The first local surgeon didn’t agree. Cole wasn’t taking "no" for an answer. She got another opinion, and this surgeon told her there was a specialist at the University of Utah, Huntsman Cancer Institute who might be willing to try what she wanted. The surgeon was willing, though he warned she might not get the result she hoped for. The care team there told her she didn’t have to have both breasts removed, and though Cole was still nursing her son from her right breast, she remained firm in her decision of a bilateral mastectomy.
Claiming her place in the ‘options game’
At 38, 12 weeks after giving birth to her healthy son and two weeks before Christmas, Cole underwent bilateral nipple-sparing mastectomy. This time, her doctors said she must undergo chemotherapy treatment. This cancer type was more aggressive than the first time.
She agreed and soon began what was to be a 12-week-long course with the chemotherapy drug Taxol. But at week six she developed what her doctors feared might become a life-threatening reaction, and her care team recommended she stop chemotherapy and complete a year-long course of treatment with Herceptin.
Through this process Cole again was a fierce advocate for herself. Determined that she did not want to be pitied as the “mom undergoing cancer treatment,” she researched and found a product called Penguin Cold Cap that cancer patients use during chemotherapy to retain their hair. It worked for her, though her doctors were skeptical.
“I didn’t have a lot of support with that decision,” she said. “Honestly, I’m just a pain. No doctor wants to have me as a patient. But I got what I wanted and I’m happy I did. I couldn’t bear that juxtaposition of having this brand new, perfect little chunky monkey on my hip and people looking at me like I’m dying. No one knew about my diagnosis other than people close to me.”
Women who’ve been pregnant and cared for their newborns can relate to the mass of hormones coursing through one’s body and the toll they can take on psychological wellness. Imagine that coupled with a cancer diagnosis, bilateral mastectomy, chemotherapy and more. How does one manage?
“Well, I put my head down. I was vocal every step along the way. I just focused on getting it done and I tried not to let it consume me too much. I was coming to terms with the fact that I was only going to be able to have this one baby. I needed to get through my treatment so that I could enjoy the good again, to get back to that good place again.”
The good place did come - shortly after completing treatment she and her significant other were married.
As before, Cole began taking the estrogen-interrupter drug Tamoxifen, and as before she began experiencing severe symptoms within a few months. This time, she opted for a hysterectomy.
Irrepressible, undaunted, advocate for cancer patients
“Now I feel great! Now I am Wonder Woman! I am forged in steel. It’s like - okay, how many times do you have to put that iron back in the fire? Because ultimately what does it do to you? How does your life story in the end affect you and how do you cope and deal with it?"
“Maybe it took me a little bit longer to get here, but I am so grateful. I feel as though in terms of where I am mentally and physically and my outlook on life, that I am forever in service to help cancer patients. No matter where I am, helping cancer patients is going to a part of my story,” Cole says.
“I want others to know that it’s okay to ask all the questions and take up all the time and say ‘Wait a minute! This is what I want. How can we work in what I want as I go through these really horrible things that no one ever wants to go through?’ I may not have a choice to go through this, but I can do it my way, and I can do it in a way that makes me feel empowered.’”
"No matter what," Cole says, "even if you’ve been given a car to build and all you have is a screwdriver, every cancer patient can find other tools. It’s about asking for help, reaching out, sharing with others. If you can find the words to say what you need and to ask for people to help you find it, that will make all the difference. That, and a compassionate doctor and a cancer care navigator.”