Choose to
protect your
health

Get an annual mammogram
Breasts may not be a comfortable topic of conversation, but talk leads to action and action is how we manage our breast health and save lives.
Get help scheduling a mammogram
Breast screening is covered by insurance
Commercial health insurers in Nevada are required to cover annual mammograms and other diagnostic imaging (like ultrasound for dense breasts) at no cost to the patient.
Here’s the uncomfortable truth
In the United States, breast cancer is the most commonly diagnosed cancer in women. The good news is women have a way to fight back. Regular breast cancer screening — like mammograms and breast ultrasounds — is the best way to find breast cancer early when it is easier to treat. Here are three reasons you should get screened.

Breast screenings can detect breast cancer before you can feel a lump. Knowing what’s normal for you, whether it’s through monthly self-exams or just noticing any change, is important. So is the early detection that a screening provides. It’s not one or the other. For the best outcome, it’s both.
Breast cancer has a 99% cure rate when detected early. Annual mammograms can’t prevent you from getting breast cancer, but they can give you the best chance of surviving it.
Early detection reduces the risk of needing a mastectomy. When breast cancer is detected early, it is often possible to remove all cancerous cells with a procedure called a lumpectomy, rather than having to remove the entire breast.
You don’t need a family history of cancer to be at risk. There is a myth that a family history of breast cancer is the most significant risk factor for an individual to get breast cancer. That simply isn't true. 85 – 90% of cases involve no prior family history of breast cancer.
Sources
- Journal of American Medical Association
- American Cancer Society
- Food & Drug Administration
- National Breast Cancer Foundation
- National Breast Cancer Coalition
- Susan G. Komen
- BreastCancer.org
- Breast Cancer Now
- Centers for Disease Control and Prevention
This material supported by Nevada Division of Public and Behavioral Health through Grants # NU58DP007102-02 and # 1NH750T000092-01-00 from the CDC.
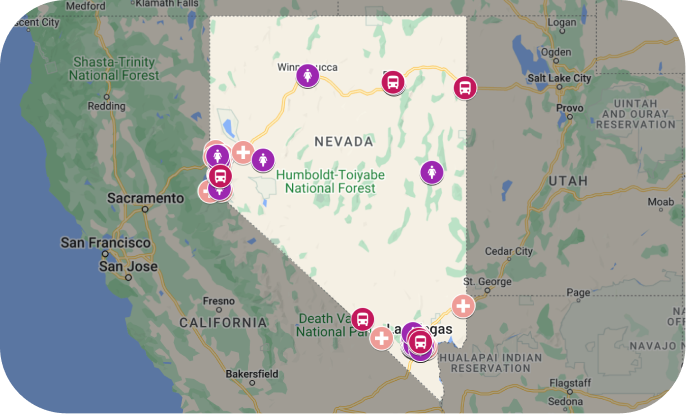
Where to Get Screened
The Risks for
Rural Women

If you don't get screened, you can't catch cancer early
Studies show that rural women get mammograms less often than other groups and, as a consequence, they are more likely to have a late-stage breast cancer diagnosis. Get an annual screening so you can catch breast cancer when it's most treatable.
Access to mammogram services and providers
Because of the scarcity of healthcare facilities in rural communities, rural women often don’t get an annual mammogram, putting their health at increased risk. We can help. Our navigator team can connect you with screening services and even help you find a primary care provider if you need one.
Change the odds
Develop your own screening plan
While most women will begin annual screening at age 40, all women should develop a screening plan with their provider based on their risk factors. Those with known risk factors may want to begin screening even earlier. Talk to your doctor about your screening plan.
Supplemental screening may be necessary
Women who have dense breast tissue may need supplemental screening (typically a breast ultrasound) as well. Speak with your doctor about your risk factors, including race, and if you should get a supplemental screening.
Most insurers in Nevada, including Medicaid, are required to cover all supplemental screenings at no cost.
Facts About Breast Cancer and Mammograms
Getting screened annually can help find breast cancer earlier when it’s easiest to treat and survive. Don’t let bad information, like these common myths, get between you and your health.
What to Expect When
Getting a Mammogram

What is a mammogram?
A mammogram is an X-ray of the breast. A mammogram offers a view of the breast that can show abnormalities before they are apparent to you or your doctor. Some facilities offer a 3D mammogram, which combines multiple breast X-rays to create a 3-dimensional picture of the breast.
How does it feel?
Some women find mammograms uncomfortable, some even find them painful, and for others, the procedure doesn't bother them at all. No matter what your experience, know that the technician is trained to provide gentle care, and any discomfort will last only a few seconds.
The procedure
On the day of your mammogram, don’t apply deodorant, antiperspirant, powders, lotions or perfumes on or under your breasts or underarms as these can cause white spots on the image.
You’ll need to remove your top and bra, so wearing a skirt or pants may be easiest. The facility will give you a gown to wear. You’ll also want to remove necklaces and any large earrings and pull back longer hair.
Be sure to tell your radiology technologist if you have noticed any changes to your breasts, have implants, are breastfeeding or might be pregnant. Also, let them know if you have trouble standing or holding still for 30 seconds at a time.
To get a high-quality picture, your breast must be compressed for a short period. You'll stand in front of the machine and the technologist will position your breast on the machine. A plastic upper plate is then lowered to compress your breast while the technologist takes an X-ray.
Generally, two views of each breast are taken for a screening mammogram. For some women, such as those with larger breasts or implants, more images may be taken. The technologist will help you change position so your breast is compressed at a different angle before another X-ray is taken. The machine may move in an arc if you are getting a 3D mammogram.
The procedure typically takes less than 20 minutes, with actual breast compression lasting only 10–15 seconds for each image.
Free and Low-Cost Mammograms
No insurance? Underinsured? No problem. Several programs in Nevada provide free mammograms to those who are uninsured, cannot afford screening, and may not qualify for Medicare or Medicaid coverage.
Do you prefer one-on-one help getting a mammogram? Contact Nevada Cancer Coalition’s ThriveNV support team by calling 775-451-1670 ext 106.
Or complete this form.