USPSTF Releases Final Research Plan for Cervical Cancer Screening
03 March, 2022
The U.S. Preventive Services Task Force in mid-March provided an update on its progress in reviewing and potentially updating its ratings for screening for cervical cancer. The final research plan—completed following a monthlong public input period and internal review—is the second step in the four-step review process and will be followed by a draft recommendation then a final recommendation.
Based on the key questions the task force will review, the group is looking to evaluate the effectiveness of different screening methods and intervals for cervical cancer screening. In the evaluation they’ll look at, among other things, modes of collection, patient compliance, and variations based on age, gender, race, ethnicity or HPV vaccination status.
A few things stand out in this review based upon the key questions and the research approach. The second question to be reviewed is: What is the test accuracy of and adherence to self-collected high-risk HPV vaginal samples?
Self-collected, at-home HPV tests are already available in the United States from some wellness companies, but they aren’t yet approved by the Food and Drug Administration for clinical use.
“We believe at-home HPV testing is the future, but at this point, we would not recommend doing home testing,” says gynecologic oncologist Kathleen Schmeler, M.D. in an interview with M.D. Anderson Cancer Center.
Some concerns with at-home testing have to do with the tests’ accuracy based on self-sampling. In a clinical setting, a medical professional would collect a sample from a woman’s cervix, but in a self-collected sample the collection is taken from the vagina. However, some argue that at-home sampling helps women to overcome barriers related to speculum examination, which can include sexual trauma, cultural beliefs, or gender identity. It may also increase access for those with structural barriers to screening.
A study by Australian researchers found, “With the emergence of HPV-based primary screening, the option of self-collection (where the woman takes the sample from the vagina herself) may overcome [these barriers], given that such samples when tested using a PCR-based HPV assay have similar sensitivity for the detection of cervical pre-cancers as practitioner-collected cervical specimens.”
Self-collected samples have found to compare favorably with physician-samples in HPV testing in low-resource and developing countries, according to a study by Indian researchers, however a German researcher found sensitivity and specificity was lacking in self-collected samples.
Should self-collection kits and methods be refined, and tests improve in specificity and sensitivity, we could see at-home HPV testing to be a cervical cancer screening option similar to how at-home stool testing is performed for colorectal cancer screening. We’ll be sure to provide updates as USPSTF makes progress on this recommendation.
You May Also Like

April 2025 Awareness Month Materials
03.28.2025
April is the awareness month for both Head & Neck cancers and Testicular cancer.

NCC Travels I-80 Educating Nevadans on Cancer
03.24.2025
Every March the team from Nevada Cancer Coalition hits the road, traveling along Interstate 80 to attend the popular Humboldt General Hospital Hea
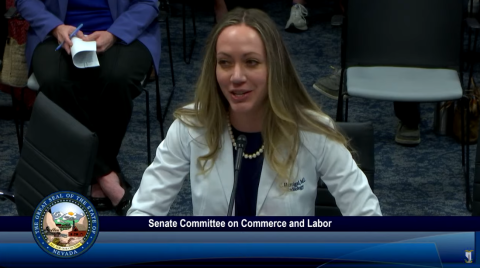
Lung Screening Bill Receives Support at Nevada Legislature
03.21.2025
A bill to improve access to lung cancer screening with low-dose computed tomography (LDCT) received support on Friday, March 21 from a number of s